The Centers for Medicare & Medicaid Services (CMS) released its proposed 2026 Medicare Physician Fee Schedule (MPFS) on July 14, 2025, and for the first time in years, it includes a headline increase to physician reimbursement. While this top-line figure may suggest relief, radiologists should take a deeper look.
Under the surface, CMS has proposed structural adjustments, particularly to work RVUs and practice expense methodology that will likely erode net reimbursement for imaging services. APS Medical Billing has reviewed the proposed changes to identify the key implications for radiology groups.
Visual Summary: How the 2026 MPFS Impacts Radiology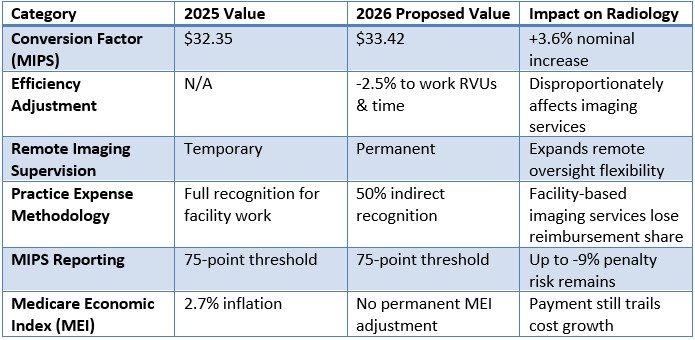
Bottom line: Most radiology practices will see pressure on revenue despite a nominal conversion factor increase, due to cuts in how imaging service resources are valued.
Efficiency Adjustment: A Blunt Instrument for Imaging Services
CMS proposes applying a 2.5% "efficiency adjustment" to nearly 9,000 services, mostly non–time-based CPT® codes. For radiology, this includes core procedures across diagnostic and interventional modalities.
The rationale: CMS believes physicians gain efficiency over time. However, organizations like the ACR argue that imaging has become more complex, with advanced reconstructions, higher data volumes, and increased documentation demands. Applying a flat cut ignores this reality and risks undervaluing modern imaging care.
Permanent Remote Imaging Supervision
In a positive move for radiologists, CMS proposes making permanent the policy allowing for direct supervision of diagnostic tests via real-time audio-video technology. This supports hybrid workflows and broader geographic flexibility, particularly valuable for teleradiology and remote site coverage.
Practice Expense Methodology: Facility-Based Penalties
CMS also proposes recalibrating the indirect practice expense methodology. In short:
• Facility-based services (e.g., hospital, imaging centers) will only have 50% of their physician work recognized in the indirect cost formula.
• This shifts payment toward office-based services and away from facility-based specialties like radiology.
Estimated impact:
• Facility-based physician payment: -7%
• Non-facility-based payment: +4%
Radiology practices tied to hospitals or imaging centers will feel this shift most acutely.
MIPS: Reporting Burden Persists
The Merit-based Incentive Payment System (MIPS) retains its current 75-point threshold to avoid up to a -9% penalty. While radiology groups often leverage registries like ACR's National Radiology Data Registry (NRDR) to meet quality metrics, the administrative burden remains high.
Small and independent radiology groups—especially those not integrated into larger health systems—are more likely to face MIPS penalties. The ACR and AMA continue to advocate for reform to reduce compliance costs and improve fairness.
ACR Perspective: Long-Term Threats Remain
The American College of Radiology (ACR) has been vocal in its opposition to efficiency-based cuts and the lack of structural reform in Medicare payment. Since 2000, inflation-adjusted physician payment under Medicare has declined 33%, while hospital payments have grown with inflation.
The widening payment gap has pushed many independent radiology groups to consolidate or align with hospitals, often at the cost of local access and practice autonomy.
Despite a nominal increase in the conversion factor, the 2026 MPFS proposal poses meaningful risks to radiology reimbursement. The efficiency adjustment and practice-expense redistribution disproportionately affect imaging services, particularly those delivered in facility settings.
APS Medical Billing continues to advocate for fair valuation of radiology services and will keep our clients informed as CMS finalizes the 2026 rule.
If you have questions about how these proposed changes may impact your reimbursement, or would like help modeling your exposure under the new rule, please reach out to your APS Practice Manager. We are here to help you protect your revenue and navigate these changes with confidence.
CPT copyright 2024 American Medical Association. All rights reserved.

