On July 14, 2025, the Centers for Medicare & Medicaid Services (CMS) released the proposed 2026 Medicare Physician Fee Schedule (MPFS). While the overall proposal includes modest increases in the conversion factor, deeper analysis reveals that pathology and other facility-based specialties may actually see net decreases in Medicare reimbursement.
APS Medical Billing has closely reviewed the proposed rule and identified the provisions most relevant to pathologists. This white paper outlines those impacts and offers insights to help your practice prepare for the changes ahead.
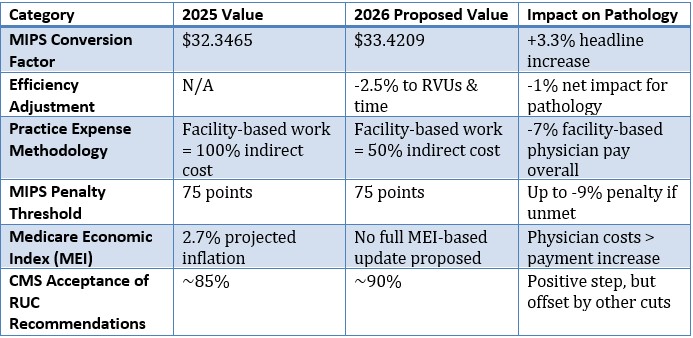
Key Takeaway: A Headline Increase, but Real-World Reductions for Pathology
Although CMS proposes a general increase in the conversion factor for 2026, two major policy changes, efficiency adjustments and practice expense redistributions, are expected to negatively affect facility-based specialties, including pathology.
Visual Summary: How the 2026 MPFS Affects Pathology
Efficiency Adjustment: Pathology in the Crosshairs
CMS proposes a 2.5% "efficiency adjustment" to work RVUs and physician time, based on the assumption that physicians have become more efficient over time. This adjustment affects nearly 9,000 services and applies broadly to pathology.
While time-based services and most telehealth codes are exempt, the majority of pathology procedures are not, making this a hidden cut despite the higher conversion factor.
Practice Expense Realignment: Penalizing Facility-Based Care
In a second major shift, CMS proposes reducing the indirect practice expense weight for services performed in facilities by half, effectively shifting reimbursement from facility-based providers to those in office settings.
Projected impact:
• Facility-based provider pay: -7%
• Non-facility-based provider pay: +4%
Many pathology groups may face even greater reductions depending on procedure mix and site-of-service profile.
MIPS and Small Practice Risk
The Merit-based Incentive Payment System (MIPS) remains a source of concern for independent pathology groups. While the penalty threshold remains at 75 points for the 2026 performance year, data from 2025 shows:
• 29% of solo practices received a MIPS penalty
• 13% of small practices received the maximum -9% penalty
• Rural and independent providers are disproportionately penalized
Diminishing Role of Physician Input
CMS is moving away from physician survey data as the foundation for RVU assignments and physician time, asserting that this input may be inflated. This shift threatens to undervalue pathology services, where procedural complexity and effort are not always apparent in claims data.
Physician societies, including the AMA, are pushing back, citing concerns over flawed assumptions and a potential decline in accuracy and fairness of reimbursement policy.
Conclusion: Navigating a Shifting Landscape
The 2026 proposed rule marks a pivotal point for pathologists. While CMS touts a long-overdue increase in the conversion factor, most pathology groups should prepare for flat or declining reimbursement as a result of:
• System-wide efficiency assumptions
• Site-of-service redistributions
• Stagnant baseline updates despite inflation
APS Medical Billing will continue monitoring developments and provide guidance to support informed decision-making for pathology groups nationwide.
Questions? Contact Your APS Practice Manager
If you have questions about how these proposed changes may impact your specific practice, or if you’d like support modeling your exposure under the 2026 rule, please reach out to your APS Practice Manager. We are here to help you stay informed, prepared, and financially secure.

