The VA Community Care Network (VCCN) is comprised of 5 Regions across the US. Depending on which VA Region providers perform services determines which claims processor is utilized for their claims. While there are 5 Regions, there are two payers which adjudicate VCCN claims, Optum Serve and Triwest Healthcare Alliance. Below is a map of the VCCN Regions and which payers adjudicate each region.
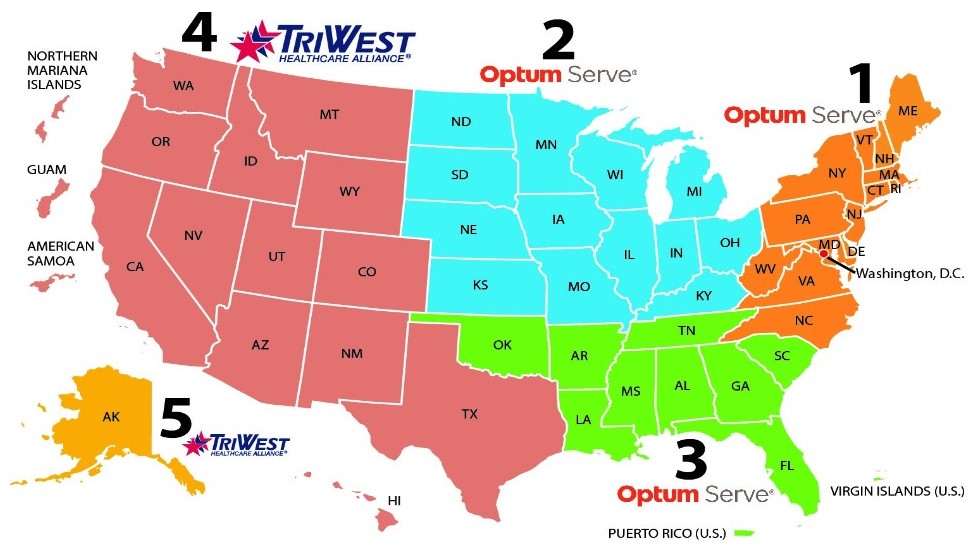
VA.GOV Region Map 1
(https://www.va.gov/COMMUNITYCARE/providers/Community_Care_Network.asp, 2023)
VCCN claims are required to have a prior authorization for services that are not connected to the Veteran’s service-connected disability or Special Authority.
(https://www.va.gov/COMMUNITYCARE/providers/prct_requirements.asp, n.d.)
Due to this requirement, VCCN will no longer process claims that are not performed at a VA hospital location without the authorization for service listed on the claim when filed. In the past, the VCCN network has been more lenient on this rule, but these guidelines have now been strictly enforced.
APS is internally reviewing and working to ensuring the authorization is on initial claims, to prevent delays in claim submission and processing by the VA. APS will continue to review, and when appropriate an APS Practice Manager and/or Client Representative may be reaching out to request the prior authorizations be added to the electronic files.

